
It is now almost 3 weeks since my beautiful little girl Harlow was born, and a good time to share my birth story.

Induction
My induction was booked for Monday 8th February when I was 38 weeks and I was required to attend hospital 3 days prior for a covid test. I then had to isolate until the induction day. Drew and I arrived at the hospital at 9am and were shown to a private room which was a nice surprise.
On the ward all the staff were in full PPE and I wore a mask each time they entered my room.
After checking in a midwife introduced herself and checked the baby’s position. There was a look of worry on her face before she explained that she thought the baby was breech, she then called a consultant to scan me. Luckily the scan confirmed that baby was head down..a huge relief!
My induction officially started at 12pm. I was given a stretch and sweep followed by my first pessary. I was then instructed to walk about as much as possible and use the exercise ball in the room to encourage movement. By 6pm nothing had happened, so I was given another pessary. I started experiencing some mild cramps around midnight which then disappeared.
I was then checked in the morning where my midwife told me that I was now 2cm dilated and could have my waters broken but there was a 48 hour wait for a delivery suite due to how busy the hospital was and because they had to adhere to strict social distancing. Drew left shortly afterwards to pick Amber up with the plan to come back once I was ready to move to the delivery suite.
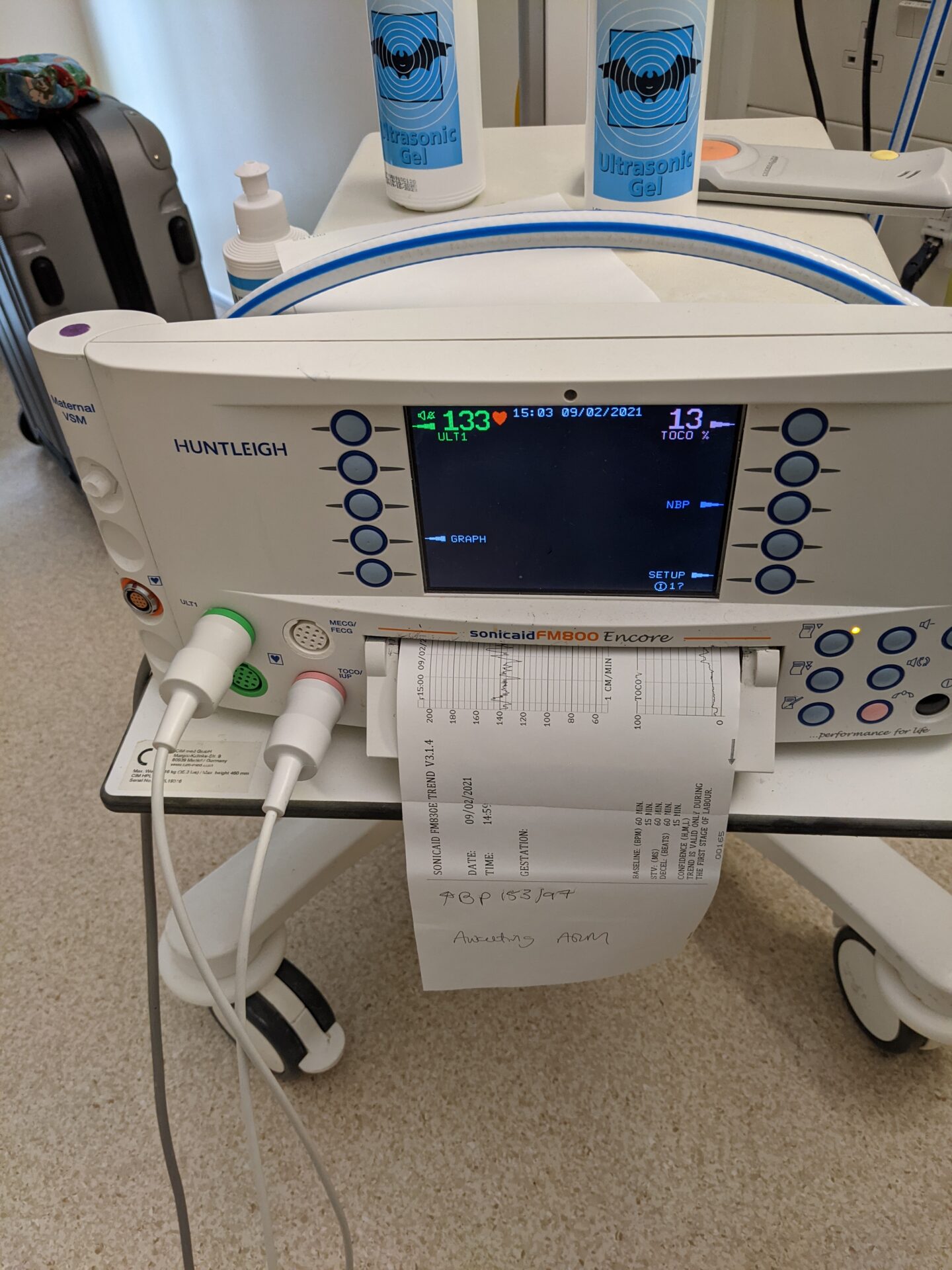
My blood pressure became a concern on the Tuesday which meant I was constantly monitored, including every few hours through the night. I was put on medication and baby was monitored on the CTG. A consultant came in to check on me and said that if my blood pressure got any higher or if I developed swelling or a headache I would be moved for delivery asap. Luckily none of those symptoms developed. So over the next few days I chilled, read and tried to keep as active as possible. I treated myself to a daily decaf Costa from downstairs and took advantage of the downtime.
Drew and Amber popped in to see me everyday but as kids weren’t allowed inside the hospital I had to meet them outside the entrance for a cuddle and a catch up. I’ve never ever been away from Amber, so seeing her even for just 15 minutes a day was lovely.
I was given another Covid test on the Tuesday morning, inline with the hospital’s guidelines to test patients every few days.
Delivery
On Thursday 11th February I was finally woken up to have my waters broken. My blood pressure had been high all night and at 3am I started to develop a headache, so was moved up the list as priority. I packed my bags ready to be moved to a delivery suite, I think this was around 6.30am, and I then called Drew to make his way to the hospital. There was a delay of an hour for the room as it needed to be thoroughly cleaned and the midwives were changing over to day staff.
Once in the delivery suite my midwife went over my birth plan, which was quite basic. Pain relief was to be gas & air and then diamorphine once the contractions get too bad to cope with. I also wanted delayed cord clamping due to being anaemic in my third trimester and antibiotics due to Amber having had group B Strep. The anaesthetist popped in to do my antibiotics and at around 10.30am the first attempt was done to break my waters, the midwife couldn’t do it so my consultant took over. I was then hooked on to the hormone drip at lunchtime on a low setting. The baby’s heartbeat was erratic so they had to keep the setting low for as long as possible, but this meant that things weren’t progressing. At 7pm the new midwife examined me and said that my front waters had been broken but my hind waters were still intact, so she broke them and the same time increased the setting on the hormone drip. I had very mild contractions which the gas & air was coping with. At 9pm the drip was increased again, once baby’s heartbeat has stabilized and at 10pm I requested diamorphine as the contractions were getting stronger.
As I was pushing baby was getting really distressed and the emergency button was pushed. By the time the Drs came in the baby was seconds away from coming out and it took a few seconds for anyone to notice. Harlow was born at 00.58 at a tiny 6lbs 2oz.
I then had issues with my placenta being unable to be delivered, a few Drs tried and I was losing a lot of blood (2 litres to be exact).
I was prepped to be moved to theatre for the manual removal of the placenta. I had to have a spinal anaesthesia which I hated as it made my legs numb for 2 hours with only a pins and needles type sensation. I also had stitches done at the same time. The whole experience made me so anxious and there was so much emphasis on how much blood I had lost. I was given a blood transfusion and then moved to a recovery room.

The staff were all incredible. The anaesthetist was the same one who did my antibiotics in the morning and he put me at ease so much, as well as checking in on during the recovery, as did a few of the theatre staff. I think I made a big impression on them with my panic attack in theatre! Awkward!


I stayed in hospital for two days after the birth as my blood pressure needed to be monitored and I was finally discharged on the Sunday afternoon.
I really wasn’t sure what to expect with the guidelines but everything was well organised. Positive cases were isolated away from negative cases, staff were always in full PPE and washed their hands before and after attending to you, and patients were tested every few days.